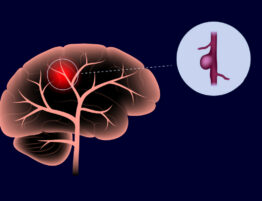
Lacunar stroke is an ischemic cerebral infarction limited to the territory of the blood supply to one of the small perforating arteries located in the deep regions of the hemispheres and the brain stem. In the process of organizing a lacunar infarction, a rounded cavity is formed, filled with cerebrospinal fluid – a lacuna. Lacunar infarction is a type of serious malfunction in the functioning of the brain’s circulatory system, as a result of which a small cavity begins to form in the human body in the places of localization of atrophied cerebral tissue after ischemia. The designations of such hollows were invented back in the distant 19th century.
A detailed description of the disease was given later in the mid-60s of the last century. Professor Fisher revealed its direct dependence on encephalopathy of a hypertensive nature. According to the average statistical data, a similar disease is diagnosed in approximately a quarter of all ischaemic strokes. Due to the small volumes of lesions and minimal consequences, lacunar abnormalities were considered to be of a benign class for a long time. But after some research in the field of neurology in a clinical setting, it became clear that such a disorder causes the development of cognitive deficits, a secondary stage of Parkinson’s disease, and some mental instability.
In this article, you will learn about the lacunar stroke symptoms and tell about the causes of infarct that should be avoided. In addition, we tell readers about the quick procedure for detecting a stroke, methods of its treatment, rehabilitation, and preventive measures.
Pathogens lacunar ischaemic stroke
The described disease can manifest itself as a result of a failure in the blood supply in one of the perforating vessels of the arteries. In almost 80% of lesions, the area of changes becomes the white matter of the cerebral region, located in the subcortical zone and the inner membrane, in the remaining 20% - at the base and bridge. Usually, the main reason for the progression of deformities is chronic arterial hypertension. Due to this, abnormalities begin to appear in the walls of the vascular canals. In the case of such a process, a decrease in the lumen of the artery is recorded in the patient, which entails problems in the circulatory system, which feeds a certain area of the cerebral tissues. After this, signs of ischemia and death appear in the affected lobe, and then a hole is formed in the place of the removed cells.
The primary etiological sources of the disease are:
- The chronic ailment of elastic and muscular-elastic arteries, renal failure with an increased number of creatinine in the blood cells.
- Diabetes.
- Alcohol abuse.
- Chronic stage of obstructive disorders occurring in the pulmonary apparatus.
- Infectious agents that have entered the body.
- Autoimmune diseases, etc.
How does lacunar stroke manifest?
Usually, the pathology is manifested by the rapid onset of focal manifestations within a couple of hours. But there are times when the violation proceeds in stages with a gradual increase in the number of problems (such a period can last from 72 hours to 6 days). At certain points, transistor attacks of the lacunar ischaemic nature stand out. In addition, with lacunar infarction, cerebral symptoms, disturbances in the cortical regions, and meningeal phenomena are not noticed. Consciousness remains clear and crisp. Also, the patient has the following symptoms:
- Hemiparesis.
- Sensory problems.
- Loss of the ability to independently perform a motor activity.
- Problems with the speech apparatus.
- Pelvic dysfunction.
- Pseudobulbar anomaly.
- Neurological abnormalities.
- Depressive state.
- Difficulty concentrating and remembering the information received.
- Decrease in the level of intellectual abilities.
- Inhibition of thinking.
When such phenomena are neglected, a person begins rapid progress of the disease, as a result of which the degree of cognitive imbalance begins to increase. The patient ceases to perceive any information, loss of motor reflexes is noted.
How to quickly identify ischemic stroke?
There is a quick test that can help identify an ischemic stroke. It’s called F.A.S.T:
- Face. Ask the person to smile. If a lacunar stroke occurs, one corner of the mouth will be lowered.
- Arms. Ask the person to raise both hands and hold them for 5 seconds. With a stroke, one arm drops, or a person cannot control it at all.
- Speech. Ask the person for a simple phrase. With a stroke, speech becomes slurred, illegible.
- Time. Call an ambulance as soon as possible.
A concept called “Time is the brain” is proposed in the WHO recommendations. Its essence is simple: the sooner a patient with a lacunar stroke is provided with medical care, the higher the chance to preserve the maximum possible number of brain cells and, as a result, restore most of the functions.
It is essential to recognize the symptoms of lacunar ischemic stroke in time and seek emergency medical attention. Patients themselves do not always recognize the signs of a stroke. Therefore, the responsibility falls on relatives and people who are nearby.
When you wait for doctors:
- Provide air access. Eliminate the pressure of tight clothing (unfasten the belt, tie). Open windows.
- Turn the person on their side in case nausea starts.
- Do not offer food or water to the person. With an ischemic stroke, swallowing is often impaired, a person may choke.
- Memorize every minute what is happening with the person so that later you can tell the doctors in detail about it. When they arrive, you will be of great help to them.
- Stay close until the doctors arrive. Talk to the patient and observe the connectedness of speech.
After the ambulance arrives:
- Describe the exact time and order of onset of symptoms.
- Report the patient’s chronic diseases (hypertension, diabetes mellitus, myocardial infarction).
- Tell us about drug intolerance, as well as the medications the patient is taking.
- It is advisable to prepare all medical documents before the ambulance arrives: extracts from the medical history, insurance policy.
During transportation, the patient will receive emergency assistance if necessary:
- restoration of normal breathing;
- lowering blood pressure;
- relief of seizures;
- prevention of cerebral edema;
- resuscitation measures.
Classification of lacunar infarct
This violation of cerebral circulation is subdivided depending on the vessel in which the blood supply basin of the brain the catastrophe occurred. In total, there are two vascular basins: carotid and vertebrobasilar. Thus, there are two types of cerebral infarction:
- lacunar infarction in the area of basal structures – occurs when blood flow in the vertebrobasilar basin is disturbed;
- a heart attack in the region of the cerebral hemispheres – appears when the carotid circulation is disturbed.
Why is lacunar stroke dangerous?
Since lacunar stroke is characterized by its own, in most cases, asymptomatic course, its diagnosis, and therefore, timely treatment, is often difficult, leading to complications. Among the main consequences of lacunar cerebral infarction, there are those that occur in the short term after a heart attack (the first six months) and more distant consequences.
- In the first six months, there may be a progression of vascular disorders with the development of a more severe stroke, repeated lacunar strokes.
- Among the more distant consequences that develop several years after an episode of lacunar stroke, the most common is vascular dementia and mental health disorders. This is manifested by sudden mood swings, changes in behavior up to the complete impossibility of self-service.
- The main outcome of lacunar infarction, which does not pose a danger, is the formation of a brain cyst. It is a circular cavity filled with liquid. Its visualization on MRI confirms a lacunar stroke suffered in the past.
Medical care for lacunar ischaemic stroke
If the patient can be taken to the hospital within three hours after the ischemic stroke, performing the thrombolysis procedure (destruction of the blood clot) is possible. The rapid elimination of oxygen starvation in the brain regions will save a significant part of the damaged tissue. An x-ray, computed, or magnetic resonance imaging is prescribed to determine the volume of brain damage.
Lacunar ischaemic stroke therapy can be divided into several main areas:
- Medication. Aimed at improving blood circulation in the affected area, thinning blood, relieving cerebral edema, maintaining heart activity, correcting glucose levels;
- Oxygen saturation of the blood. Oxygen therapy is performed if the blood is less than 92–95% oxygenated. If this does not help, the patient is transferred to mechanical ventilation;
- Patient care measures – correct body position, adequate nutrition and drinking regimen, prevention of pressure sores, bandaging of limbs, care for catheters, artificial respiration apparatus, massage, and gymnastics;
- Prevention of complications, including pneumonia, urinary tract infections, blood clots.
Even with the timely provision of emergency measures for the treatment of ischemic stroke, only one in three patients fully recovers. Rehabilitation is indicated to increase the chances of recovery (or partial return of lost functions).
What are the consequences of ischemic stroke?
After the transferred lacunar stroke, the following develop:
- movement disorders: paresis (partial paralysis), weakness, heaviness in the limbs (usually on one side of the body), loss of fine motor skills, loss of facial expressions on one or both halves of the face;
- decreased sensitivity;
- speech disorders: slurred speech, difficulty in choosing words, misunderstanding of others;
- visual impairment: black spots, general deterioration of vision, double vision;
- cognitive impairments: decreased attention, memory, reduced speed and quality of thinking, writing and reading disorders;
- emotional disorders, depression.
The negative consequences of an ischemic stroke depend on the extent of the brain damage, as well as on the location of the damaged area.
Rehabilitation after a lacunar stroke
Treatment of the consequences of ischemic stroke can be divided into several directions:
- Movement restoration (classes with a physical therapist, aqua therapy, training on simulators, the use of modern techniques: Bobath therapy, Exart, PNF method);
- Returning independence in everyday life (classes with ergoteparevt in a specially equipped training apartment);
- Recovery of speech and swallowing;
- Drawing up a menu with the recommendations of the attending physician;
- Blood pressure control and drug therapy;
- Hygiene procedures (including ostomy care and removal of ostomy);
- Symptomatic treatment (prevention or treatment of pressure ulcers, pain relief, etc.);
- Restoring control of the pelvic organs;
- Treatment of depressive conditions with the help of a psychologist.
The rehabilitation program is carried out in three stages:
- The first stage begins from the first days after the postponed lacunar ischemic stroke. At the same time, the possibilities of active rehabilitation are limited since the patient is in bed and is inactive. The patient is turned over, he is given a massage, and breathing exercises are assisted. It is essential to communicate with the patient even if their own speech is impaired or unable to respond. The perception of speech affects the functioning of the functional areas of the brain and positively affects the emotional and physiological state of a person.
- The second stage lasts up to several months after the lacunar stroke. It can take place both directly in the hospital and in a specialized rehabilitation center. During this period, massage, therapeutic exercises, physiotherapy are prescribed. Specialists work on speech and cognitive functions (memory, thinking, imagination). This stage can last up to six months: it all depends on the severity of the stroke.
- In the late third rehabilitation period, active methods are used to restore functions and skills. Fine motor skills and self-service skills are restored. It is also important to develop a patient’s commitment to rehabilitation activities and a positive attitude.
At all stages of the program, a key principle is an individual approach to each patient. In some cases, one or two rehabilitation courses are enough (the patient is discharged with detailed recommendations and a set of exercises to be performed at home).
Stroke remains an urgent topic for research: new rehabilitation methods, effective drugs, and treatment regimens appear regularly. Therefore, our specialists take training courses on a mandatory basis, participate in scientific events and publish their research data.
Lacunar ischaemic stroke prognosis
The prognosis for the development of lacunar stroke with timely diagnosis is favorable, characterized by rapid and complete recovery. However, recurrent strokes and multiple lesions reduce the chances of full recovery. There is data where described a mean annual stroke rate between 4% and 7%, 1511 an early (24 months) cumulative recurrence rate between 7% and 14%, and a late (48 to 72 months) cumulative recurrence rate between 26% and 34 %.
Many are also interested in the question: is it possible to work with lacunar cerebral infarction?
During the treatment and rehabilitation period, it is worth abandoning increased mental and physical exertion, as this can lead to a recurrence of a heart attack or the development of further adverse consequences (dementia, mental disorders).
It can be concluded that such, at first glance, an insignificant pathology, such as a lacunar stroke, can lead to irreversible consequences in the absence of timely diagnosis and treatment. Therefore, neurologists and radiation diagnosticians should give this pathology special attention, and a person who has felt the symptoms listed above should not postpone but immediately seek qualified help.
Prevention of lacunar stroke
A healthy lifestyle should be ensured to prevent the formation of even the smallest gaps as a consequence of a lacunar ischaemic stroke, including the following recommendations:
- Control your diet by excluding foods with a high content of cholesterol, sugar, and other harmful substances;
- Take prophylactic drugs that strengthen the walls of the vessels of the brain;
- Monitor blood pressure and older people are recommended to measure it several times a day;
- Make it a rule to keep a diary of pressure readings. Take measurements in the morning, on an empty stomach, then after a meal, and at night, before going to bed;
- Of course, ecology, smoking, and alcohol also bring lacunar infarction closer. It would help if you rested in nature more often and give up bad habits;
- Rest and moderate work should be the foundation of your lifestyle. Do what pleases you, do not let stress. Do not overwork and do not “test” the work of the heart with excessive physical exertion. Too much sport is also harmful;
- Aspirin is considered good prophylactic medicine, as well as reducing the risk of re-disease – vascular infarction. It should be taken in a pure, preferably soluble form;
- Finally, do not be lazy once a year to conduct an MRI of the brain and an examination for disruption of the activity of small, deep vessels. And then such a phenomenon as a heart attack, in general, will seem impossible to you.
Unfortunately, not only people in old age are susceptible to this disease. Even mature and young men (in 55% of cases) and women (in 45%) are prone to lacunar ischaemic stroke. The main reason lies in a stressful and unfavorable lifestyle, excessive stress on blood vessels, heart, and brain neurons. Therefore, consult a doctor immediately if you have already suffered a similar illness, and the first symptoms of a stroke made themselves felt. Caution, in this case, will not be excessive.














Please, leave your review
Write a comment: