Neurofibromatosis is a genetic disorder in which tumors destroy tissue connections. This pathology most affects the skin. But sometimes, the tumor can also affect the bones of patients. The main cause of this disease is a genetic predisposition. Although sometimes it can appear all of a sudden. According to statistics, neurofibromatosis affects one newborn per three and a half thousand. Another name for the neurofibromatosis type is Recklinghausen’s disease.
A neurologist makes a diagnosis based on a review of the patient’s current condition. They also look at the results of several tests. Often, doctors, detect neurofibromatosis when two or more of the typical signs are inherent:
- Large numbers of light brown pigmented spots;
- Elevated pigmentation;
- Advanced neurofibromas;
- Bone abnormalities.
At present, it is impossible to cure the disease completely. Thus, treatment is symptomatic only. Neurofibromatosis often affects the central and peripheral nervous systems. It causes neurofibromatosis of the auditory nerve and meningiomas. This disease has many risk factors. One of the most dangerous is the disruption of vital body functions. Because it can be fatal. Read more about the causes and symptoms of neurofibromatosis.
What is Neurofibromatosis?
Neurofibromatosis is a group of diseases with typical clinical manifestations. Tumors develop on nerve tissue. It is a result of a series of hereditary diseases called neurofibromatoses. The diseases are accompanied by the appearance of benign, less often cancerous tumors. They affect:
- Skin;
- Internal organs;
- The central and peripheral nervous system;
- Subcutaneous tissue;
- Spinal cord roots.
The German pathologist Friedrich Daniel von Recklinghausen first described neurofibromatosis types. He studied the disease for a long time.
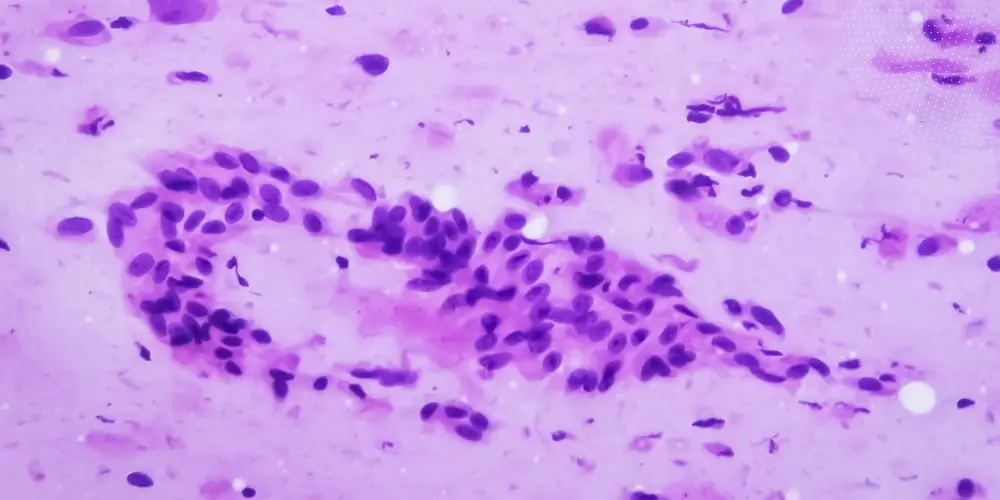
The cytological nature of neurofibromas is Schwann, nerve, and mast cells. Depending on the stage of the disease, doctors distinguish the following signs of neurofibromatosis:
- The initial stage is in which flat pigmented spots form on the child’s back and limbs.
- In the bone changes stage, there is a deformation of the patient’s bone tissue.
- At the tumor stage, doctors find neurofibromas and gliomas on the skin and soft tissues.
- At the stage of organic change. There is a disturbance in the functioning of the neighboring organs.
Sometimes juvenile myelomonocytic leukemia accompanies neurofibromatosis in children. It is a malignant disease of the blood and bone marrow. Doctors often have these clinical cases. Although the change of benign neoplasms, doctors diagnose infrequently.
Signs of Neurofibromatosis
Often, the first sign of the disease is flesh-colored spots on the body that resemble coffee and milk. These are not the only symptoms that state neurofibromatosis. As signs of neurofibromatosis are:
- Café-au-lait spots;
- Neurofibromas;
- Axillary freckling (freckles in the armpit area);
- Lisch nodules (benign tumors on the iris of the eye);
- Optic glioma (a tumor of the optic nerve);
- Macrocephaly (abnormally large head);
- Short stature;
- Learning disabilities;
- Scoliosis (curvature of the spine);
- Abnormal skeletal changes.
Benign tumors – neurofibromas – can also appear because of which the disease gets its name. The main problem is that such tumors can change and become dangerously malignant. It happens under the influence of certain factors.
In some cases, neurofibromatosis type manifests only as symptoms of various chronic diseases. Despite this good neurologists can easily determine the diagnosis of the pathology.
All these signs can show such a serious disease as neurofibromatosis. There are main neurofibromatosis types 1 and 2 of this disease. There are also four more types. Read about them further in the article.
I Type
Doctors characterize neurofibromatosis type I by:
- Pronounced clinical polymorphism;
- A progressive course;
- Many organ involvements;
- High frequency of complications, including those resulting in death:
- development of cardiopulmonary failure due to marked skeletal anomalies;
- malignant degeneration of neurofibromas, etc.
The variety of somatic mutations in different tumors in type I patients is striking. It is the main difference between neurofibromatosis 1 and 2. According to the current opinion, it is the reason for the phenotypic polymorphism. Neurofibromas are in the superficial and deep soft tissues of various localizations:
- In the axillary regions;
- On the thighs;
- On the buttocks;
- In the deep soft tissues;
- In the ocular region;
- Mediastinum, retroperitoneum;
- On the tongue;
- On the gastrointestinal tract and other areas.
They impair the function of neighboring organs when localized in:
- Mediastinum;
- Abdomen;
- Orbit.
They also have an increased risk of malignancy.
II Type
Neurofibromatosis type II results from damage to a gene localized in chromosome 22. People inherit it, like Neurofibromatosis type I, in an autosomal dominant way. You also need to know the difference between neurofibromatosis 1 and 2.
Doctors characterize the disease by the presence of various neoplasms in the CNS. Bilateral schwannoma of the vestibulocochlear nerve (VIII cranial nerve) is the most common. It appears even with minimal cutaneous and extraneural symptoms. Also, other concomitant diseases occur:
- meningiomas;
- astrocytomas;
- peripheral nerve lesions, and other types of tumors;
- cataracts.
Doctors have not identified any orthopedic abnormalities in type II. Neurofibromatosis type 2 occurs at a rate of 1 per 40,000 to 50,000.
III Type
Type III is like type II in many ways. But an important distinguishing feature is the presence of a neurofibroma. As a rule, they occur on the palms. In this type, the development of symptoms occurs between the ages of 20 and 30.
IV Type
Multiple neurofibromatosis lesions in the skin are typical symptoms of type IV disease. There is a high risk of developing optic nerve glioma and neurolemma. In this type, cutaneous neurofibromas prevail over other manifestations of the disease.
V Type
Neurofibromatosis type V is like type I. Doctors characterize it as unilateral changes. They are typical of neurofibromatosis type I. Since they occur only in one or more segments of the skin. Neurologists believe it results from mutations in the postzygotic stage.
They are capable of affecting any dermatome. Most cases are sporadic, although physicians have noted familial signs of neurofibromatosis as well. People with other abnormalities are extremely rare. Still, the affected segments can have:
- Lisch nodules;
- Pseudarthrosis.
Neurologists divide segmental NFM into four subtypes. Only one of which is genetically determined. Brown-colored patches usually represent skin changes. But eventually, neurofibromas can appear. Other complications of Neurofibromatosis do not occur. The prognosis is favorable.
VI Type
The sixth type of disease has almost no manifestations. The only sign is skin pigmentation. It can be very abundant. As a rule, this type is diagnosed in people aged 20-35. It has the most favorable prognosis. Lethality is extremely low in this type of neurofibromatosis.
Neurofibromatosis Causes
Only two roots of neurofibromatosis causes are accurately known:
- A hereditary factor;
- Spontaneous mutation factor.
In the first case, the presence of the disease affects all cells of the body without exception. That is, cellular elements multiply, and tumors appear. Also, the pathology causes serious pigmentation disorders. Many spots appear for no clear reason. Today, this condition is not fully understood. Thus, it is quite difficult to single it out as a separate group.
Multiple neurofibromatosis is an autosomal dominant disease. If a person inherits even one copy of a defective gene, they will still develop the disorder. If only one parent has neurofibromatosis, the children have a 50% chance of the disorder.
The severity of the disease can vary depending on the gene’s expression level. About half of the cases of the disease arise through spontaneous mutations. That is, the disease can occur in people who have no family history of the disease. The number of males and females affected by neurofibromatosis is about the same.
Complications of Neurofibromatosis
In 10% of cases, neurofibromas transform into malignant tumors. The high-risk group includes patients with a long follow-up history. Pregnant women should be wary of signs of neurofibromatosis. Six percent of children have impaired mental development. They have problems mastering learning skills (reading, writing, counting).
Such children have trouble remembering new information. They also take a long time to adapt to unfamiliar situations. Patients of all ages are susceptible to depression. Because they experience discomfort, shame, and embarrassment due to their disfigured appearance.
Multiple neurofibromatosis provoke:
- Endocrine disorders;
- Epileptic seizures;
- Muscle hypotonia;
- Renal and pulmonary artery stenosis;
- Changes in pigmentation. Increased pigmentation system with the active division of melanocytes. These are cells with a large amount of melanin. In some patients, the disease may manifest in the presence of characteristic spots. More than five spots of pigment spots with a diameter of 5 to 15 millimeters is a great danger. It is a high probability of having neurofibromatosis types;
- Pulmonary cysts;
- Interstitial pneumonia;
- Clitoral hypertrophy;
- Risk of thyroid and adrenal tumors;
- Appearance of tumors in the form of “lumps” under the skin;
- Bone deformities;
- In some cases, neurofibromatosis causes severe mental retardation;
- Abnormalities in the development of the gastrointestinal organs.
Doctors should check any changes in the appearance, size, and number of neurofibromas. Changes can show malignant tumor growth. The earlier malignant changes are detected, the higher the chance of successful treatment outcomes.
People with NF1 have an increased risk of developing other forms of malignancy in neurofibromatosis types:
- Breast cancer;
- Leukemia;
- Brain tumors;
- Certain types of soft tissue malignancies.
Risk Factors of Neurofibromatosis
The most common risk factor is nerve exposure to neurofibrosis. Neurofibromas with exophytic growth (outward) cause aesthetic discomfort to the patient, while those growing inward lead to compression of the nerve and surrounding tissues, causing pain. They also threaten to impair the vital functions of the body.
Patients with neurofibromatosis have an increased risk of developing some forms of malignant tumors. Sometimes, multiple neurofibromatosis leads to death. Doctors considered the most reliable risk factors for deformity progression to be:
- Cobb angle;
- Rotation of the apical vertebra more than 11°;
- The festooned symptom.
The latter can be expressed very roughly, with the formation of the so-called two-toothed beak. Such a vertebral body deformity is a reliable risk factor for the progression of spinal deformity.
Timely contact of parents with a doctor in case of suspected neurofibromatosis in the child allows for early diagnosis of the disease, monitoring of the child according to clinical guidelines, and prescribing treatment if necessary. You can learn more about all stages of the program at a consultation with a geneticist.
A Word from Lone Star Neurologists
After reading this article, you are more familiar with these neurofibromatosis types. If you find similar symptoms in yourself, contact our Lone Star Neurology clinic. We have the best professionals in the field of neurology. We will be able to advise you and find the most appropriate solution for the problem you have.
FAQs
- Is neurofibromatosis painful?
As a rule, this disease does not bring severe pain. But, discomfort is very likely. People with neurofibromatosis can get an education, work, and live a normal life.
- Is there a cure for neurofibromatosis?
No, at the moment, there is no cure for this disease. But, people can receive supportive therapy. It is excellent for suppressing symptoms.
- Can neurofibromatosis be cured?
In some cases, surgery can help. Even though Recklinghausen’s neurofibromatosis is a genetic disease. Thus, if the symptoms of neurofibromatosis interfere with your life, see your doctor as soon as possible.
- When do symptoms of neurofibromatosis begin?
Most often, clinical signs are café-au-lait spots on the body, in the folds of the knee and elbow joints. They appear in 1-3 months of a child’s life. Further, voluminous skin formations develop. Neurological abnormalities appear or are absent depending on the location of the neoplasm.










Please, leave your review
Write a comment: