Neuroinflammation is a complex process. It involves the activation of defense cells within the brain. This process has emerged as a significant factor. It contributes to many neural and psychiatric disorders.
In a healthy brain, the immune system functions to protect against infections and injuries. However, continuous or excessive activation of them leads to inflammation. It can damage brain cells and disrupt neural networks. The prevalence of mental illness has prompted researchers to investigate the underlying mechanisms. The studies have highlighted the role of neuroinflammation in the progression of these issues.
Understanding the relationship between neuroinflammation and brain health is vital. This way, we can gain valuable insights into the pathophysiology of these diseases. This article will delve into the key aspects of this phenomenon and its impact on health. In our article, we will:
- Examine the molecular mechanisms.
- Talk about the role of different cells in the brain.
- Consider the link between neuroinflammation and specific health diseases.
- Discuss the potential therapeutic implications of targeting neuroinflammation.
The Link Between Inflammation and Mental Health Disorders
Neuroinflammation can disrupt the delicate balance of neurotransmitters and neural circuits. When immune cells become overactive, they release inflammatory cytokines. It can damage brain cells, impair synaptic plasticity, and trigger degenerative processes. These alterations can contribute to the development and progression of various mental disorders.
The prevalence of mental conditions has been steadily increasing worldwide. According to the World Health Organization, depression is the leading cause of disability. It affects millions of people. Anxiety illnesses are also highly prevalent, impacting people of all ages. Moreover, inflammatory markers have been found to be elevated in people with these conditions. It suggests a strong link between inflammation and health.
Numerous studies have demonstrated a significant association between inflammation and mental disease. For instance, people with depression often exhibit increased levels of inflammatory markers. They are C-reactive protein (CRP) and interleukin-6 (IL-6). Similarly, people with anxiety disorder have elevated levels of inflammatory cytokines. These findings suggest that inflammation may play a crucial role in the pathogenesis of these conditions.
Inflammation and Depression: What the Research Says
Several mechanisms have been proposed to explain the link between inflammation and depression. Inflammatory cytokines can impair neurogenesis. It’s the process of generating new neurons in the brain, which is essential for mood regulation. Also, inflammation can disrupt the hypothalamic-pituitary-adrenal (HPA) axis. It’s a system involved in stress response. It leads to dysregulation of stress hormones.
The recognition of the role of inflammation in depression has opened up new avenues for intervention. Anti-inflammatory drugs have been explored as potential adjunctive treatments for depression. They include non-steroidal anti-inflammatory drugs (NSAIDs) and omega-3 fatty acids. Furthermore, lifestyle modifications can help reduce inflammation and improve health. They include regular exercise and a healthy diet.
The Role of Inflammation in Anxiety Disorders
Anxiety and inflammation are closely connected. Chronic inflammation can contribute to the development and exacerbation of anxiety disorder, by affecting various brain regions involved in fear and anxiety processing. Inflammatory cytokines can increase neural activity in the amygdala. It’s a brain region associated with fear and anxiety. It leads to heightened anxiety responses.
Traditional treatments for anxiety conditions are effective for many people. However, addressing the underlying inflammatory component may offer additional benefits. Anti-inflammatory medications, mindfulness-based stress reduction techniques, and lifestyle interventions that promote a healthy immune system can be valuable adjuncts to standard treatments.
Neuroinflammation and Stress: A Complicated Relationship
Stress, a ubiquitous aspect of modern life, can have profound effects on both physical and brain health. One of the key mechanisms through which it impacts well-being is by inducing neuroinflammation. This complex interplay between stress and inflammation can contribute to mental disease
When people experience chronic issues, their bodies release stress hormones such as cortisol. Prolonged exposure to elevated cortisol levels can dysregulate the immune system. It leads to increased production of inflammatory cytokines. These inflammatory molecules can:
- Damage brain cells
- Impair synaptic plasticity
- Disrupt neural networks involved in mood regulation and cognitive function during inflammation
The bidirectional relationship between stress and inflammation is evident in the exacerbation of mental disorder. Chronic stress can trigger or worsen conditions like depression and anxiety, by promoting neuroinflammation. Conversely, people with mental disorders may experience heightened stress responses. It further fuels the inflammatory process.
A combination of lifestyle changes and therapeutic interventions can be beneficial to mitigate the negative effects of stress-induced neuroinflammation. Regular physical activity, mindfulness practices, and adequate sleep can help reduce stress levels. Also, diet can help regulate inflammation.
In cases of severe mental condition, pharmacological interventions may be necessary. Antidepressants, anti-anxiety medications, and antipsychotics can help alleviate symptoms and reduce neuroinflammation. However, it is important to note that these medications may have side effects. And you must use them under the guidance of a healthcare professional.
Chronic Inflammation: A Catalyst for Mental Health Disorders
Chronic inflammation has emerged as a significant factor leading to mental condition. This condition arises when the body’s immune response remains elevated for extended periods, often due to lifestyle factors, dietary choices, and underlying health conditions.
Long-term inflammation can have a detrimental impact on brain health. Inflammatory markers are cytokines and chemokines. They can disrupt the delicate balance of neurotransmitters. They can impair synaptic plasticity and damage brain cells. These alterations can lead to:
- Cognitive deficits.
- Emotional dysregulation.
- Increased susceptibility to mental illness.
Research has uncovered a strong association between:
- Chronic inflammation.
- A range of mental conditions.
Studies have shown that depression often exhibits elevated levels of inflammatory markers. They are C-reactive protein (CRP) and interleukin-6 (IL-6). Similarly, anxiety disorder and bipolar disorder have increased inflammatory activity in the brain.
Moreover, emerging research suggests a link between chronic inflammation and schizophrenia. Inflammatory processes may contribute to the development of:
- Psychotic signs.
- Cognitive impairments associated with this disorder.
The exact mechanisms underlying this connection are not fully understood. However, it’s believed that inflammation may disrupt neurodevelopmental processes. And it can contribute to abnormal brain connectivity.
Understanding the role of chronic inflammation in health is vital. Thus, we can explore potential interventions to mitigate its effects. Lifestyle modifications can help reduce inflammation and promote mental well-being. Also, emerging research suggests that targeting specific inflammatory pathways may offer novel therapeutic approaches for treating mental conditions.
Future Directions: Neuroinflammation Treatment Strategies
Our understanding of neuroinflammation’s role in mental disorders continues to grow. So, too do the potential treatment strategies. A multifaceted approach combines pharmacological interventions and lifestyle modifications. It holds promise for addressing the underlying inflammatory processes and improving patient outcomes.
Emerging Therapies:
- Anti-inflammatory Drugs. Traditional anti-inflammatory medications are non-steroidal anti-inflammatory drugs (NSAIDs) and omega-3 fatty acids. They promise to reduce neuroinflammation and alleviate symptoms of mental disease. However, further research is needed to optimize their use and minimize potential side effects.
- Novel Therapeutic Agents. Researchers are exploring the development of novel drugs. Those specifically target inflammatory pathways involved in mental disorders. These agents may offer more targeted and effective treatments with fewer side effects.
- Lifestyle Interventions. Lifestyle modifications include regular physical activity, a healthy diet, and stress reduction techniques. They can significantly impact neuroinflammation. These interventions can help regulate the immune system. They can reduce oxidative stress and promote brain health.
Neuroinflammation and Anxiety: Research Opportunities:
- Precision Medicine. Identifying biomarkers of neuroinflammation could enable personalized treatment approaches. They can be always tailored to every patient’s needs. By understanding the specific inflammatory pathways, clinicians can select the most appropriate interventions.
- Gut-Brain Axis. The gut microbiome plays a crucial role in immune function and inflammation. Research into the gut-brain axis may reveal new therapeutic targets, for modulating neuroinflammation and boosting health.
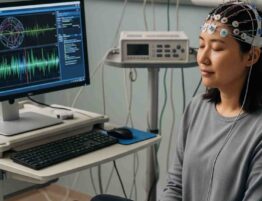
- Neuroimaging Techniques. Advanced neuroimaging techniques help visualize brain inflammation and track the effects of treatment. These tools can aid in the development of more effective therapeutic strategies.
Neuroinflammation has emerged as a key player in the pathogenesis of various mental diseases. By addressing the underlying processes, we can develop more effective treatments. A mix of pharmacological interventions, lifestyle changes, and emerging therapies holds promise for improving the lives of people affected by chronic inflammation and mental health issues. Continued research is essential. to fully understand the relationship between neuroinflammation and health and to develop innovative tactics for prevention and treatment.
However, no matter what the health case is. Regular monitoring is essential. We recommend choosing a reliable healthcare provider. Choose us as your trusted partner. Our team of experienced professionals is ready to provide comprehensive and personalized care.
What sets us apart?
- Expert Care. Our skilled physicians and specialists offer a wide range of services to address your health needs.
- Patient-Centered Approach. We focus on your comfort and well-being. We tailor treatment plans to your unique circumstances.
- State-of-the-Art Facilities. Our modern clinic has the latest technologies to ensure accurate diagnoses and effective treatments.
Convenient Access. We offer flexible appointment scheduling and convenient online services to make everything accessible.












Please, leave your review
Write a comment: