Susceptibility to migraines is influenced by multiple factors. Genetic and hormonal factors play an important role in migraine development. The environment is also vital. Genomic studies have identified 13 genetic variants. These variants are strongly linked to migraine susceptibility. These genes affect glutamatergic neurotransmission and synapse function. The biological processes underlying migraines are complex and require careful study. Scientists have evaluated the link between the brain and the gut bacteria.
Research has demonstrated that disruptions in gut health can trigger headaches, and effective solutions are being developed. A balanced microbiome may help prevent headaches. A review study from Norway revealed a significant correlation. Patients with gastrointestinal diseases are more likely to have migraines. These people suffer from reflux, constipation and diarrhea. This happens even after adjusting for patient characteristics. Understanding these key connections between gut health and migraines may help improve treatment approaches.
How Gut Bacteria Affect Neurological Disorders, Including Migraines
Gut bacteria play an important role in various neurological conditions. This relationship functions as a complex communication network. This relationship creates an important connection between the digestive system and the brain. This connection is crucial in determining how gut health influences brain function. These disruptions can affect neurological functions, including the onset and severity of migraines.
How do intestinal bacteria affect neurological disorders? Let’s explore:
- Biochemical Pathways: Gut microbes produce neurotransmitters such as serotonin and dopamine. These neurotransmitters influence mood and pain perception. An imbalance in gut bacteria can alter neurotransmitter levels. This imbalance can potentially trigger migraines and affect emotional well-being.
- Inflammation Responses: The gut lining may become compromised. Harmful substances can enter the bloodstream, leading to systemic inflammation. This inflammation may reach the brain, causing headaches or exacerbating migraines. Inflammation activates pain pathways.
- Immune System Modulation: The gut microbiome helps regulate immune function. Imbalanced gut bacteria prompt an overactive immune response. This response leads to inflammation that may trigger migraines or worsen existing symptoms.
- Gut-Brain Signaling: The vagus nerve directly connects the gut and the brain. The vagus nerve transmits signals that affect mood and pain perception. An imbalance in gut bacteria can disrupt these signals, impacting migraine frequency and intensity.
- Toxin Production: Some bacteria produce metabolites that negatively affect the central nervous system. These metabolites can contribute to headache development and other neurological symptoms.
Gut bacteria play a vital role in neurological disorders. This connection emphasizes the importance of maintaining a healthy microbiome. A healthy microbiome can be supported through diet, probiotics, and lifestyle adjustments. This connection highlights the potential for innovative treatments targeting gut health to help manage and alleviate migraine symptoms.
The Impact of Inflammation Response on Migraine Triggers
The inflammatory response is critical to understanding the causes of migraines. There is growing evidence pointing to gut health as a significant factor. Disruptions in gut bacteria can lead to chronic inflammation. It may trigger or worsen migraine episodes. Recent research highlights the gut-brain communication pathway as a key player in this connection. It sheds light on how microbial imbalances impact brain function and pain perception.
Here’s how the inflammatory response affects migraine:
- Gut Dysbiosis: An imbalance of gut bacteria can compromise the intestinal lining, allowing harmful substances to enter the bloodstream. This imbalance triggers an immune response. This process can result in chronic inflammation that impacts the central nervous system.
- Pro-inflammatory cytokines: Altered gut microbiota may increase the production of these immune signaling molecules. Pro-inflammatory cytokines can cross the blood-brain barrier and activate pain pathways. These cytokines can contribute significantly to migraine development.
- Neuroinflammation: Chronic inflammation in the brain can sensitize neurons, exacerbating pain perception. This makes migraines more frequent and severe.
- Vagus Nerve Signaling: Inflammatory signals traveling through the vagus nerve can amplify the brain’s response to pain, linking gut health to headache intensity.
This understanding is crucial for recognizing the link between inflammatory responses and migraine triggers. It offers promising insights into new treatment strategies focusing on gut health to reduce migraine severity and frequency.
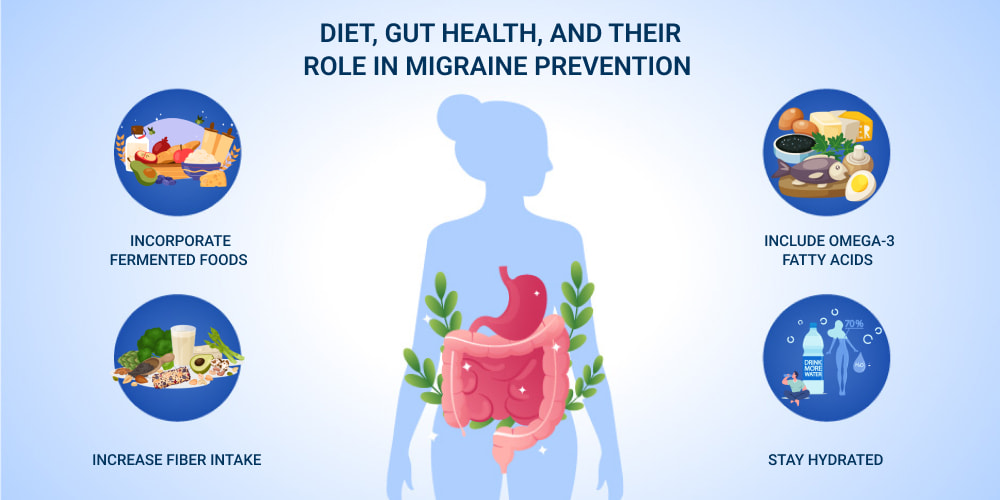
Diet, Gut Health, and Their Role in Migraine Prevention
Maintaining a balanced diet is crucial for promoting health and preventing migraines. Research increasingly supports the connection between diet and migraines. Certain foods can support a healthy gut environment. Conversely, certain foods may trigger inflammation that leads to headaches. Focusing on dietary choices is vital for helping reduce migraine frequency and severity.
Here are key dietary factors to consider for migraine prevention:
- Incorporate Fermented Foods: Yogurt, kefir, sauerkraut, and kimchi are rich in probiotics that promote a diverse gut microbiome. A diverse microbiome helps reduce inflammation and support brain health.
- Avoid Processed Foods: Artificial sweeteners, preservatives, and high-sugar foods disrupt microbiome health and increase inflammation. This inflammation can potentially trigger migraines.
- Increase Fiber Intake: Whole grains, legumes, fruits, and vegetables provide prebiotics that nourish beneficial gut bacteria. This nourishment supports a balanced microbiome.
- Include Omega-3 Fatty Acids: Salmon, flaxseeds, and chia seeds reduce inflammation and also support brain function. These benefits can help alleviate migraine symptoms.
- Stay Hydrated: Dehydration can worsen migraines and disrupt gut function. Aim to drink plenty of water throughout the day.
By adopting dietary practices that prioritize microbiome health, individuals can take proactive steps to reduce their risk of migraines. This approach also helps support overall well-being.
The Science of Gut Bacteria’s Influence on the Brain: Key Research Insights
Scientific research increasingly reveals how gut bacteria influence brain function and migraines. This research sheds light on the powerful connection of the gut-brain axis. Studies focus on how gut microbes produce neurotransmitters and metabolites that impact mood and cognition. These microbes also affect pain perception. Researchers use fecal microbiota analysis and brain imaging. They also employ behavioral assessments. These techniques help researchers explore this complex relationship.
Here are key insights from recent research on gut bacteria and neurological disorders:
- Neurotransmitter Production: Gut microbes produce serotonin, dopamine, and gamma-aminobutyric acid (GABA), which regulate mood and anxiety. An imbalance in these microbes can disrupt brain chemistry. This disruption can contribute to mood disorders and migraines.
- Vagus Nerve Signaling: The vagus nerve acts as a communication highway between the gut and the brain. Disruptions in gut health can send pain signals through this nerve. These signals can link gastrointestinal disturbances to migraine onset.
- Inflammation and Immune Response: Certain bacterial strains can either reduce or promote inflammation. Chronic inflammation from gut dysbiosis can trigger neuroinflammation, leading to increased pain sensitivity and migraine attacks.
- Microbiome Diversity: A balanced microbiome correlates with a lower incidence of migraines. It also correlates with improved mental health. These correlations highlight the importance of maintaining microbiome health.
As researchers deepen their understanding of the gut-brain axis, they aim to develop innovative treatments that help alleviate migraines and enhance mental well-being.
Emerging Treatments: Using Gut Health to Manage Migraines
Emerging treatments increasingly focus on the role of gut bacteria. Improving gut health through diet and supplements helps manage and prevent migraines. Medical professionals are increasingly exploring this approach to migraine treatment. This holistic approach addresses potential root causes rather than just alleviating symptoms. It offers promising new avenues for migraine management.
Here are some emerging treatments that utilize gut bacteria to manage migraines:
- Probiotic Supplements: Introducing beneficial bacteria through probiotics helps restore gut balance and reduce inflammation that may trigger migraines. Lactobacillus and Bifidobacterium are particularly noted for their potential to reduce headache frequency and intensity.
- Prebiotic Intake: Inulin and fructooligosaccharides (FOS) feed beneficial gut bacteria and promote a healthier microbiome. Garlic, onions, and bananas naturally contain these prebiotics. These foods foster a balanced gut environment that may help address migraine causes.
- Gut-Targeted Therapies: Scientists are investigating treatments that directly modify the gut microbiome to help address factors contributing to migraines. These include fecal microbiota transplantation (FMT) and customized microbial therapies. These therapies can be customized to individual needs.
- Anti-Inflammatory Diets: Focusing on fatty fish, leafy greens, and whole grains is important. This diet helps reduce systemic inflammation. Inflammation is commonly linked to migraine onset. Reducing processed foods and additives also supports microbiome health and lowers migraine risks.
- Stress Management and Gut Health: Stress disrupts the gut-brain axis and can aggravate migraines. Integrating mindfulness, meditation, and yoga supports gut function. These relaxation techniques decrease migraine frequency.
Individuals have differences in microbiomes. This variability means that what works for one person might not be effective for another. More research is necessary to understand the long-term effects and to determine optimal dosages of probiotics and prebiotics.
As our understanding of the gut-brain axis deepens, integrating gut health into treatment plans could revolutionize migraine management. This approach may offer patients more targeted and sustainable relief.
Practical Tips for Improving Gut Health and Reducing Migraine Risk
Improving gut bacterial health can significantly reduce migraine risk. This approach helps balance inflammatory responses. Here are some practical tips to enhance microbiome health that may help minimize migraine frequency and severity:
- Adopt a Balanced Diet: Incorporate vegetables, fruits, and whole grains. These foods nourish beneficial gut bacteria. Consume yogurt, kefir, sauerkraut, and kimchi, which provide probiotics that promote a healthy microbiome. Include omega-3 fatty acids from fatty fish, flaxseeds, and chia seeds, which help reduce inflammation and support brain function. Avoid processed foods, artificial additives, and excessive sugar, which can disrupt gut bacteria balance and trigger inflammation.
- Take Probiotics and Prebiotics: Consider adding probiotic supplements to help restore gut balance. Look for Lactobacillus and Bifidobacterium, which have shown promise in migraine prevention. Garlic, onions, and bananas contain prebiotics that support healthy bacteria growth.
- Stay Hydrated: Dehydration can worsen migraine symptoms. Drink plenty of water throughout the day. Adequate water intake supports both hydration and microbiome health.
- Manage Stress: Practice yoga, meditation, and deep breathing to help reduce stress. Chronic stress can negatively impact gut health. Stress is a known contributor to migraine development.
Incorporating these tips may help reduce migraine frequency and severity. Consider consulting with healthcare professionals who specialize in gut health and neurology for personalized guidance.












I've given up... the stress her office staff has put me through is just not worth it. You can do so much better, please clean house, either change out your office staff, or find a way for them to be more efficient please. You have to do something. This is not how you want to run your practice. It leaves a very bad impression on your business.
Please, leave your review
Write a comment: