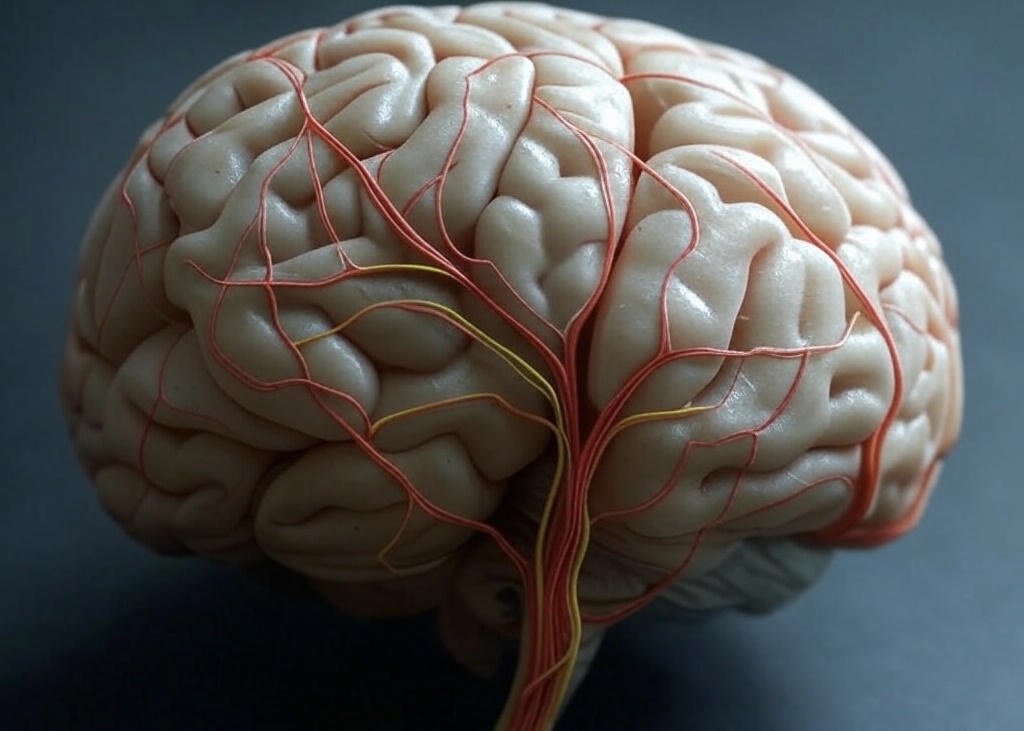
How Anxiety and Neuropathic Pain Are Linked – A Neurological Insight
Anxiety and neuropathic pain share a deep and often unrecognized connection. This neurological insight reveals how the nervous system intertwines pain and emotions. The brain and spinal cord process physical sensations, while psychological health functions through overlapping pathways. When nerves are damaged or dysfunctional, neuralgia can emerge. Clinical presentation includes burning, prickling, or shooting sensations. Anxiety amplifies this ache by heightening the brain’s responsiveness to discomfort, typically creating a chain reaction. Cortisol further intensifies nerve signaling. This stress hormone makes pain feel worse.
Conversely, persistent pain can trigger nervous tension. Persistent discomfort wears on emotional resilience. In this article, we’ll provide crucial information about how LoneStarNeurology specializes in unraveling these complex connections. We offer expert care tailored to neuralgia and mental health. Our neurologists use cutting-edge diagnostics and personalized plans. They break the pain-anxiety loop and help patients regain control. At LoneStarNeurology, we address the nervous system holistically. We provide solutions that restore comfort and calm, transforming lives.
When the Nervous System Crosses Wires: Pain and Emotion
The nervous system is the body’s command center. It processes physical pain and emotions like anxiety. When these signals overlap, it’s like wires crossing, amplifying discomfort. This neurological insight explains why chronic pain and anxiety often feed each other. The brain and nerves share pathways. Misfiring or heightened sensitivity can turn fleeting pain into persistent suffering. Here’s how the nervous system creates this pain-emotion loop:
- Shared Pathways: The brain’s amygdala and insula process pain and anxiety. When you’re anxious, these areas become hyperactive. This hyperactivity makes pain signals feel stronger. This overlap can turn minor discomfort into chronic pain.
- Neurological Misfiring: Damaged or overactive nerves send faulty pain signals. For example, in neuropathy, nerves misfire, causing burning or tingling. Anxiety heightens this by keeping the nervous system on high alert.
- Feedback Loop: Chronic pain increases anxiety by disrupting daily life. In turn, anxiety ramps up stress hormones like cortisol. It inflames nerves and worsens pain. This cycle keeps the nervous system in overdrive.
- Heightened Sensitivity: Chronic stress or anxiety makes the nervous system oversensitive. This “central sensitization” lowers the pain threshold. Even small triggers like a light touch feel intense.
These overlaps show why treating chronic pain requires neurological insight. It’s not just about physical damage. Emotions play a huge role. For instance, a stressed brain may amplify a nerve injury’s impact. It makes pain feel unbearable. Put simply, it’s like a smoke detector that blares at burnt toast — the nervous system overreacts. Breaking this cycle involves calming the nerves and mind together. Cognitive behavioral therapy, medications, or nerve-targeted treatments can reset the system. Understanding how pain and anxiety intertwine is vital. We can address both, easing suffering and restoring balance.
Chronic Pain’s Emotional Toll: How Mental Health Suffers
Chronic pain, especially neuropathic, goes far beyond physical discomfort. It’s an invisible burden that deeply affects mental health. This often leads to anxiety, depression, and emotional exhaustion. Persistent pain signals can wear down the nervous system and alter brain chemistry, disrupting emotional balance and resilience. The relationship between persistent pain and psychological health is deeply interconnected and bidirectional. Persistent discomfort, especially from neuropathic pain, can trigger nervous system struggles such as anxiety, depression, and irritability.
These mental health challenges don’t just coexist with pain—they amplify it. When someone is anxious or depressed, their perception of pain becomes more intense and challenging to manage. This vicious cycle feeds into itself, making relief feel out of reach. For many individuals, this ongoing loop of physical and emotional suffering becomes exhausting. It also gets frustrating and emotionally overwhelming.
Consider these common emotional effects of chronic pain:
- Anxiety about future pain episodes: People often worry when the next flare-up will strike. It leads to constant mental tension.
- Sleep disturbances: Pain disrupts sleep, and lack of rest worsens emotional stability.
- Social withdrawal: When pain limits mobility or energy, people may isolate themselves. It leads to loneliness and an increased risk of depression.
- Hopelessness and depression: Living with no clear end to pain can drain hope and joy. It severely affects mental health.
- Loss of identity: Struggling to keep up with work, hobbies, or family roles can cause grief. It also leads to lowered self-worth.
- Irritability and mood swings: Chronic discomfort can make emotional regulation more difficult. It leads to frustration or sadness over minor issues.
- Cognitive fog: Pain and emotional stress can impair memory, focus, and decision-making.
In a real-life scenario, someone living with sciatica or diabetic neuropathy may begin to fear everyday tasks. They may struggle with routine activities like grocery shopping or climbing stairs. This fear stems not from the impossibility of completing the task, but from the possibility of sudden, severe pain or the embarrassment of stopping halfway. The anticipation of discomfort often triggers anxiety, heightening the perception of pain and creating a self-perpetuating cycle. Over time, this can lead to avoidance, isolation, and a diminished quality of life. That’s why it’s essential to address chronic pain’s physical and emotional aspects. This is essential for lasting well-being.
Managing Pain and Anxiety Together: A Smarter Strategy

Chronic pain and mental health challenges like anxiety often intertwine. They amplify each other’s impact. Integrative care offers a holistic solution, simultaneously addressing physical and cognitive symptoms. Neurologists at LoneStar Neurology combine medical expertise with psychological support. They create personalized pain management plans that improve patients’ quality of life.
Integrative care acknowledges that chronic pain is not purely a physical issue. It profoundly impacts emotional well-being, disrupts sleep patterns, and raises stress levels. This approach also recognizes that anxiety can increase pain sensitivity. Anxiety can increase pain sensitivity, making symptoms feel more intense. The mind and body are closely connected. Treating one without the other often leads to limited relief. Addressing the physical and emotional aspects together is pivotal. Neurologists and pain specialists can help patients break this cycle. They improve quality of life and promote more long-term healing and resilience. Strategies include:
- Physical Therapy: This method relieves neuropathic pain through movement while reducing dependence on medication. It also improves mental well-being.
- Medication Management: Analgesics or anti-neuralgia drugs are often prescribed alongside anti-anxiety medications in ways that minimize side effects.
- Cognitive Behavioral Therapy (CBT): Helps patients reframe pain-related thoughts and manage anxiety triggers.
- Mindfulness and Relaxation Techniques: Meditation and breathing exercises lower stress. These techniques ease pain and anxiety.
- Biofeedback: Teaches patients to control physiological responses, reducing pain and calming the mind.
- Lifestyle Adjustments: Sleep hygiene, nutrition, and exercise plans support overall health. These plans address both pain and mental health.
Professionals at LoneStar Neurology emphasize multidisciplinary care. They collaborate with psychologists, physical therapists, and pain specialists. This approach ensures comprehensive treatment. It ranges from diagnostic testing to therapy, all customized to the patient’s needs.
Addressing chronic pain and mental health together is pivotal. Integrative care empowers patients to regain control. Neurologists guide them through evidence-based pain management strategies, fostering resilience and hope. This smarter strategy alleviates symptoms and enhances long-term well-being. It proves that treating the body and mind as one is the key to lasting relief.
Why a Neurological Insight Can Change Your Treatment Plan
Chronic pain and anxiety often stem from complex interactions within the nervous system. They make neurological insight critical for effective treatment. Consulting a neurologist provides a deeper understanding of how these conditions arise. It enables tailored pain management plans that address root causes rather than just symptoms. LoneStar Neurology combines cutting-edge diagnostics with compassionate care. It offers patients a path to lasting relief.
Neurologists specialize in the nervous system. It regulates pain signals and emotional responses. Their expertise uncovers connections between chronic pain and anxiety. It is something general practitioners might overlook. Neurologists craft precise, individualized treatment plans by identifying specific neurological patterns such as nerve dysfunction or central sensitization. This neurological insight transforms outcomes. It reduces symptoms and improves quality of life.
LoneStar Neurology has advanced diagnostic tools, like EMG, EEG, and neuroimaging. These tools are combined with a patient-centered approach. Our team listens, evaluates, and designs comprehensive strategies. They integrate medical, psychological, and lifestyle interventions. The benefits of this approach include:
- Accurate Diagnosis: Pinpoints nervous system abnormalities driving pain and anxiety.
- Personalized Medication Plans: Optimizes drugs targeting nerve pain or anxiety with minimal side effects.
- Advanced Therapies: Offers nerve blocks, Botox for migraines, or neuromodulation. These options are essential for precise pain management.
- Behavioral Interventions: Incorporates CBT or biofeedback to address nervous system-driven anxiety.
- Holistic Support: Includes physical therapy and lifestyle changes to support nervous system health.
- Ongoing Monitoring: Adjusts treatment based on progress, ensuring long-term effectiveness.
Neurological insight is invaluable. This is because it reveals how the nervous system amplifies or sustains symptoms. For example, chronic pain may involve overactive discomfort pathways. Anxiety might reflect neurotransmitter imbalances. LoneStar Neurology’s blend of expertise and empathy ensures patients receive innovative care. Their care is rooted in science and delivered with compassion.
Choosing a neurologist for chronic pain and anxiety means choosing precision. LoneStar Neurology’s commitment to cutting-edge diagnostics and our tailored pain management empowers patients to break free from the cycle of suffering. We prove that neurological insight is the key to transformative treatment.










I've given up... the stress her office staff has put me through is just not worth it. You can do so much better, please clean house, either change out your office staff, or find a way for them to be more efficient please. You have to do something. This is not how you want to run your practice. It leaves a very bad impression on your business.
Please, leave your review
Write a comment: